When people think about cardiovascular health, exercise is often the first thing that comes to mind. Nutrition, however, plays an equally important role in supporting how the heart functions, how the body recovers, and how consistently healthy habits can be maintained over time. Everyday food choices influence energy levels, circulation, and overall heart health in ways that are often overlooked.
At Vision Elite Training, heart health is viewed as something that develops through a combination of movement, recovery, and supportive nutrition habits. Alongside structured training, nutrition guidance is available to help individuals build eating habits that align with long-term health rather than short-term fixes.
In this blog, we explore the role of nutrition in supporting cardiovascular health and why balanced, sustainable nutrition habits can make a meaningful difference when paired with thoughtful training.
Why Diet Plays a Critical Role in Heart Health
The heart is a muscle that works continuously, responding to physical activity, stress, and recovery demands throughout the day. Nutrition influences several key factors related to cardiovascular health, including cholesterol levels, blood pressure, blood sugar regulation, and inflammation.
For example, individuals who rely heavily on processed foods or skip meals may experience energy crashes during workouts, poor recovery, or difficulty staying consistent with training. Over time, these patterns can place unnecessary strain on the cardiovascular system, highlighting the well-established link between an unhealthy diet and cardiovascular disease.
Balanced Meals as the Foundation
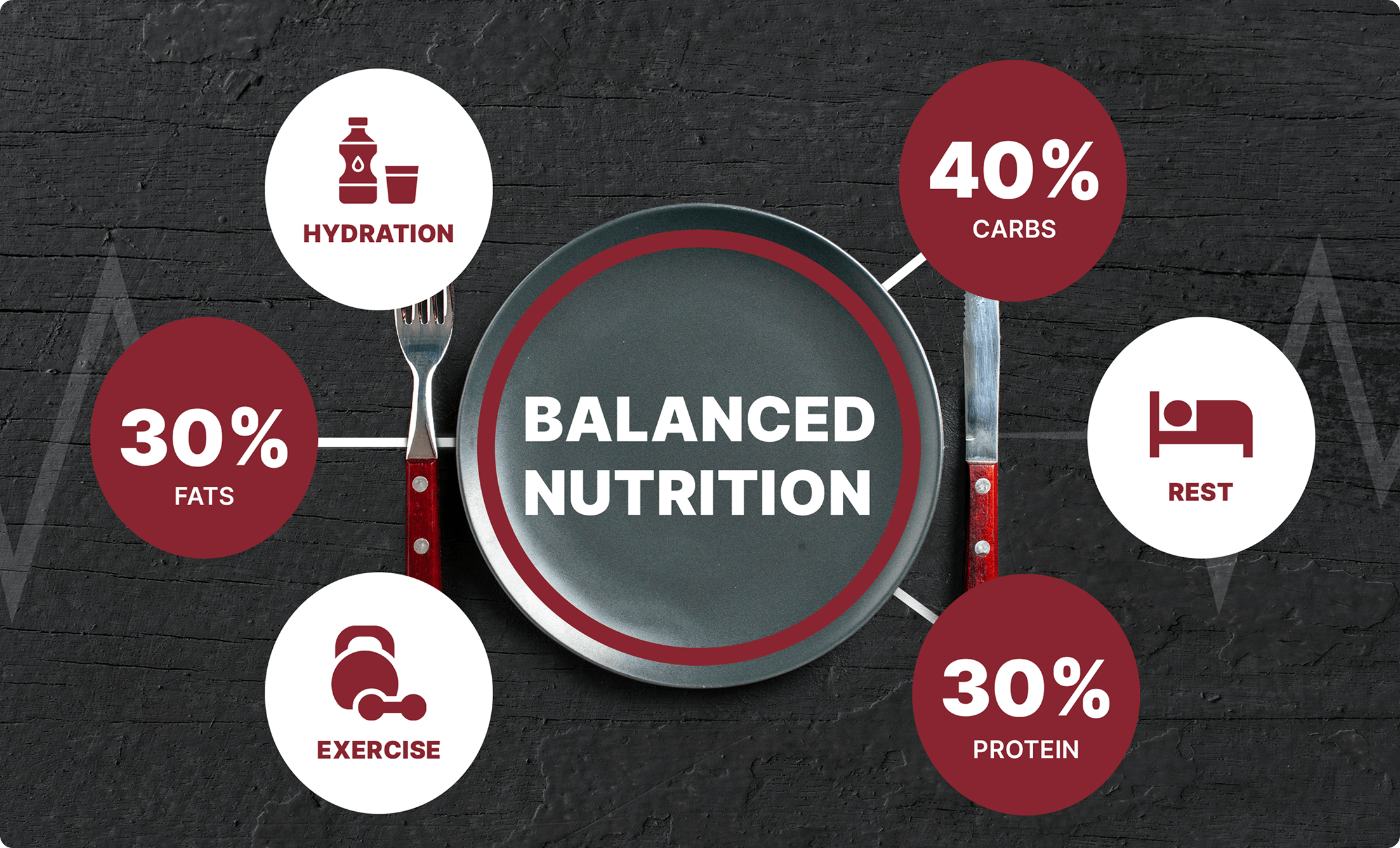
A balanced approach to nutrition supports cardiovascular health by providing the body with the nutrients it needs to function efficiently. Rather than isolating individual foods, balanced meals emphasize how different nutrients work together to support heart health.
Whole Grains and Fiber
Whole grains such as oats, brown rice, and millets are rich in fiber, which plays an important role in heart health. Fiber helps lower LDL cholesterol levels by reducing absorption in the bloodstream and supports digestion and gut health.
Fiber also helps regulate blood sugar by slowing the absorption of carbohydrates, which can improve insulin sensitivity and support healthier blood pressure levels. Including whole grains regularly supports steadier energy throughout the day and more consistent training performance.
Fruits and Vegetables
Fruits and vegetables provide essential vitamins, minerals, antioxidants, and fiber that support cardiovascular function. Antioxidants help reduce oxidative stress, while fiber supports cholesterol management and blood pressure regulation.
A practical way to approach this is by including a variety of colors on the plate. Different colors often represent different nutrients, so eating a range of fruits and vegetables helps ensure a broader intake of heart-supportive compounds. This variety supports heart health while keeping meals enjoyable and sustainable.
Healthy Fats and Cardiovascular Support
Not all fats affect heart health in the same way. Healthy fats, such as omega-3 fatty acids found in fatty fish and walnuts, help reduce inflammation and support healthy triglyceride levels. These fats also contribute to the maintenance of healthy blood vessels.
Monounsaturated and polyunsaturated fats, found in foods like olive oil, avocados, nuts, and seeds, are associated with lower LDL cholesterol and higher HDL cholesterol levels. Including these fats as part of balanced meals supports heart health without the need for restrictive eating patterns.

Evidence-Based Eating Patterns That Support Heart Health
Research consistently shows that long-term eating patterns matter more than short-term diets when it comes to cardiovascular health. Several evidence-based dietary approaches have been associated with improved heart health markers, including cholesterol levels, blood pressure, and overall cardiovascular risk.
Rather than promoting one “perfect” diet, these approaches are closely aligned with established dietary guidelines that support heart health and pair well with regular training and recovery.
Mediterranean-Style Eating
The Mediterranean-style eating pattern emphasizes whole, minimally processed foods and healthy fats. It includes generous amounts of fruits, vegetables, legumes, nuts, and whole grains, with olive oil as a primary fat source. Red and processed meats and added sugars are limited.
This approach has been linked to a lower risk of coronary heart disease and protective effects against vascular inflammation. For individuals who train regularly, this style of eating also supports steady energy levels and recovery through nutrient-dense foods.
DASH Diet (Dietary Approaches to Stop Hypertension)
The DASH diet focuses on fruits, vegetables, whole grains, and lean protein sources such as fish, poultry, and nuts. It also emphasizes reducing sodium intake and limiting sugary beverages.
This eating pattern has been shown to be effective in lowering blood pressure, improving lipid profiles, and supporting healthy weight management. For many people, DASH principles align well with structured training programs by supporting hydration, recovery, and cardiovascular efficiency.
Plant-Based and Flexitarian Approaches
Plant-based and flexitarian eating patterns prioritize fruits, vegetables, whole grains, legumes, and nuts, while limiting or excluding animal products. These approaches are associated with lower BMI, reduced LDL cholesterol levels, and improved blood glucose control.
When planned thoughtfully, plant-forward eating can support cardiovascular health while still meeting the nutritional demands of training. Including adequate protein and calorie intake is especially important for individuals who are physically active.
Low-Fat, High-Carbohydrate Patterns
Low-fat, high-carbohydrate dietary patterns reduce saturated and trans fats while increasing carbohydrate intake from whole foods such as fruits, vegetables, whole grains, and legumes.
This approach has been associated with reduced atherosclerotic cardiovascular disease risk and overall cardioprotective effects. For those engaging in regular movement or strength training, whole-food carbohydrates can help support energy availability and training performance.
Nutrition, Training, and Heart Health
Nutrition becomes even more important when combined with regular training. Exercise places stress on the body, and nutrition helps the heart and muscles respond and adapt to that stress.
For example, someone who trains consistently but eats irregularly may struggle with fatigue, poor recovery, or inconsistent progress. In contrast, pairing structured training with balanced nutrition supports energy levels, recovery, and long-term adherence. This combination allows the heart to adapt safely and efficiently over time.
The Role of Recovery and Fueling
Recovery is a key component of heart-healthy training, and nutrition plays a major role in this process. After exercise, the body needs nutrients to replenish energy stores, repair tissue, and bring the cardiovascular system back to a balanced state.
Consistent recovery nutrition supports the body’s ability to handle ongoing training without excessive fatigue. Over time, this helps create a sustainable approach that supports both performance and cardiovascular health.
Practical Nutrition Habits That Support Heart Health
Supporting heart health does not require drastic dietary changes. Small, consistent habits tend to have the greatest impact over time:
- Eating regular, balanced meals
- Including whole foods most of the time
- Staying hydrated throughout the da
- Avoiding extreme or overly restrictive diets
- Aligning nutrition with training and recovery needs
These habits support consistency, which is one of the most important factors in long-term cardiovascular health.
Frequently Asked Questions About Nutrition and Cardiovascular Health
Q.What is meant by nutritional management of cardiovascular disease?
It involves using consistent, evidence-based eating habits to support heart function and reduce risk factors. This includes managing cholesterol, blood pressure, and blood sugar levels through balanced meals, appropriate portion sizes, and sustainable dietary patterns rather than extreme or short-term diets.
Q.What is the relationship between cardiovascular disease and diet and exercise?
Cardiovascular disease is strongly influenced by both diet and exercise because they determine how the heart adapts to daily demands. Regular physical activity strengthens the heart and improves circulation, while nutrition provides the fuel and nutrients needed for that adaptation. When either is lacking, cardiovascular strain increases; when both are aligned, the heart functions more efficiently and disease risk is reduced.
Q.Can nutrition alone improve heart health without exercise?
While nutrition has a significant impact on heart health, the greatest benefits come from combining good nutrition with regular movement. Exercise strengthens the heart muscle, while nutrition supports energy, recovery, and adaptation. Together, they create a more effective and sustainable approach to cardiovascular health.
Q.What are the nutritional recommendations for cardiovascular disease prevention?
Nutritional strategies for cardiovascular disease prevention aim to support healthy circulation by managing fat quality, sodium intake, and overall dietary balance.
Get Heart Healthy at Vision Elite
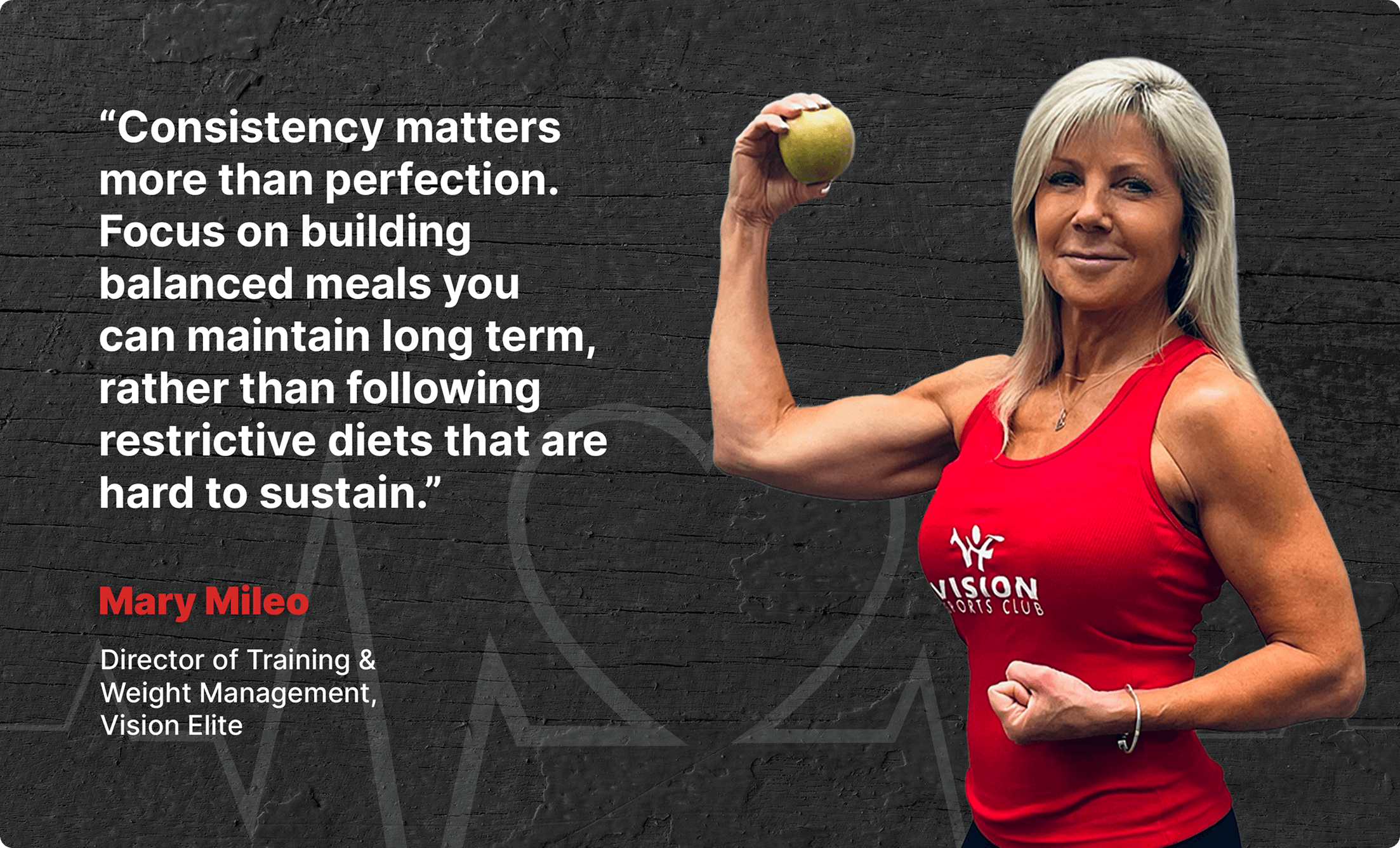
Supporting cardiovascular health is not about choosing one perfect diet or following rigid rules. It is about building consistent nutrition habits that work alongside training, movement, and recovery.
A balanced approach to eating helps support heart function, energy levels, and long-term wellbeing. When nutrition and training are aligned, the heart is better supported both during exercise and throughout daily life.
For those looking for guidance on how to align nutrition with training and heart health goals, Vision Elite Training offers support through structured coaching and nutrition counseling to help individuals build sustainable habits that fit their lifestyle.